Palliative care is about exploring what ‘quality of life’ means to that person in front of us, whose heart will take its last beat sooner than previously thought. For that person and those important to them, death is on the horizon … somewhere…
So, by a holistic assessment in any setting, by any person, we can affirm living until that last moment and we can attend to that person’s quality of life for that time,
Every second of every minute of every hour of every day matters.
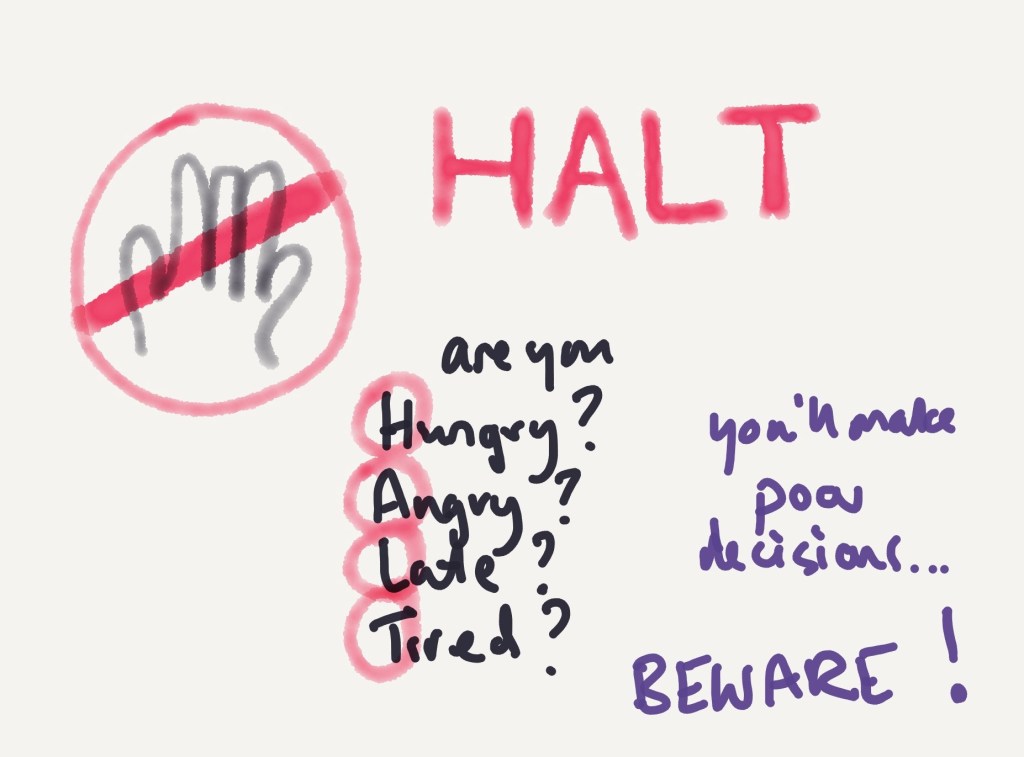
In our assessment, which could be 5 minutes or 50 minutes , we can ask what is important to that person; if they could, what would they want to be doing? How can we help?
People still are afraid that ‘palliative care’ means active dying, stopping things, stopping care, giving up – it doesn’t. Care never stops, treatments might do, especially if they are burdensome to the person and the benefit/ burden balance shifts – but care never stops. If you hear people talk about ‘ceilings of care’, please correct them… they are referring to ‘ceilings of treatment’ ie what is the absolute limit of treatment for this person? It is treatment, not care.
So, as someone providing palliative care in any setting, from any discipline, any role – dust off that metaphorical magnifying glass and get detecting!